Principles of Allocation
- There is one single national waiting list containing the data of the patients awaiting transplant.
- Any patient who is an Israeli resident, based on the recommendation of his or her physician is entitled to be included in the transplant waiting list.
- The data of all the patients awaiting transplant in Israel are stored in a computerized data bank at the National Transplant Center. The data are constantly updated and they include various medical details.
- For each organ, there is a system of allocation criteria, established according to the characteristics required for the match between the donor and the recipient (such as blood type, weight and height) and the characteristics of the organ itself from an immunological point of view (degree of the necessity of tissue match), and according to the probability of providing life quality and of saving life (data such as age, waiting period, blood test results, etc.) These criteria are inbuilt in a computer program, specifically developed for and adjusted to each organ.
- When a donor whose family has consented to the donation is found in one of the Israeli hospitals, his or her data are transmitted to the National Transplant Center and are fed into the computerized system.
- The system cross-checks the data of the donor with the data of the waiting patients and locates the patients that are the most suitable for transplant.
- The organ allocation system is egalitarian and transparent.
- The Steering Committee of the Transplant Center carries out a periodic control of the allocations and updates the allocation program according to need and to the progress in transplant technology.
- In case of dilemmas, when two or more patients that are entitled to the same extent to receive the organs have been located by the computer, the National Transplant Center seeks expert advice in order to hold a medical debate and to decide to which patient the organ shall be allocated. If no decision is made at this stage, the Transplant Center holds further consultations with additional, specially appointed experts, who are not connected to or employed by the hospitals in which the transplants are to take place. If necessary, the Head of the Steering Committee and, occasionally, even the General Director of the Ministry of Health shall get involved in the decision-making.
- Priority on the transplant list is in accordance with the priority program based on the Organ Transplant Law 5768 - 2008, Article 9(b) (4)..
Heart Allocation
Principles
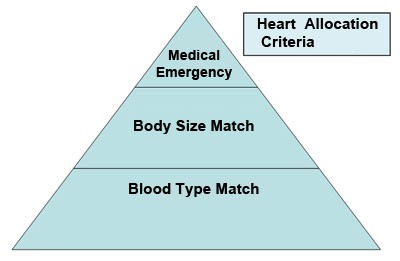
Heart allocation is done based on the match of the blood type and body weight of the donor and the recipient and on the seniority on the waiting list. The severity of the condition of the different transplant candidates is also taken into account. The waiting list is divided into two, according to the severity of the condition: Status 1 and Status 2 (see details further on).
Waiting List
There is no age limit for heart transplants.
Status 1 list: candidates in a state of emergency, including:
a. Patients hospitalized because of their severe condition, requiring medication administered by means of continuous intravenous infusion and/or pump support, or b. Patients with an artificial heart, even if they are not hospitalized permanently.
Status 2 list: the patients included in this list are waiting in their homes, in a relatively stable condition.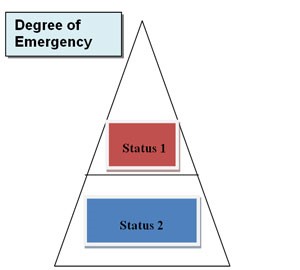
Allocation Model
When a heart for transplant is found, the blood type and body dimensions (weight and height) of the donor are entered, and the computer issues a print-out with the list of the waiting patients suitable from the point of view of their size (up to 20% more or less than the donor), while taking seniority into account (greater seniority confers priority).
Medical emergency is the first consideration in the allocation decision, for which reason the heart donation is offered first to the Status 1 waiting patients. The second consideration examined is the blood type.
The heart shall be offered first to patients with an identical blood type; the possibility of transplanting the heart into another patient in a state of emergency with a matching blood type shall be examined only if there is no emergency case in the identical blood type category and shall be subject to a match in the body dimensions of the donor and the recipient.
If there are two or more candidates suitable for the same heart transplant, the cardiologists treating these patients shall hold a consultation and shall decide upon the waiting patient in the most serious condition who shall receive the donation. If they fail to reach an agreement, an "external" cardiologist (who is not related to the hospitals in which the transplants are carried out), appointed to this effect by the National Transplant Center, shall make this decision, after having heard out the parties. In order to ensure a correct and reliable decision, the "external" physician shall visit the Status 1 emergency patients in the hospitalization departments. These visits shall take place from time to time, together with a representative of the National Transplant Center.
Lung/s Allocation
Principles
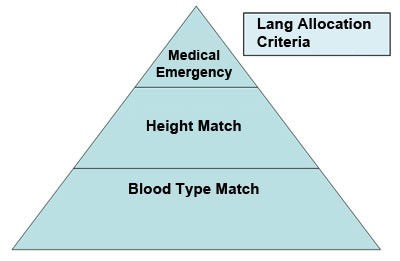
Lung allocation is done based on the match of the blood type and severity of the condition and on the height match between the donor and the recipient.
The allocation model is in conformity with LAS (Lung Allocation Score), based on: age, waiting period, type of lung disease, and lung functions, measured according to a number of parameters.
Severity of the disease: the score range (LAS) is 27-80: the more severe the medical condition, the higher is the score.
Waiting List
There is no age limit for lung transplants. Transplant candidates whose condition has deteriorated to the point where artificial ventilation is necessary and with LAS over 70 shall be entitled to receive a donation from a donor with an identical blood type, and also from a donor with a matching blood type.
Allocation Model
When a lung for transplant is received, it shall be allocated to the patient with the most severe medical condition, if there is a match between the height of the donor and the height of the recipient. Some patients require the transplant of one lung, and other patients require the transplant of both lungs.
Allocation of a Combined Heart-Lungs Transplant
The candidates are assigned to the lung donation waiting list. A candidate defined as an emergency case shall be moved to the top of the lung donation waiting list after consultation with lung specialists from other lung transplant centers. Following approval, the treating physician shall report to the National Transplant Center.
- Status 1 heart transplant candidates shall take priority over heart-lung transplant candidates.
- A heart-lung transplant candidate that has reached the top of the lung donation waiting list shall take priority over Status 2 heart transplant candidates.
Liver Allocation
Principles
There are two liver allocation models, one for adults and one for children.
Liver allocation to adults
The allocation model for adults is called MELD (Model for End-stage Liver Disease) and it is based on a mathematical formula that was developed by one of the leading transplant centers in the USA. This model was adopted by the United Network for Organ Sharing (UNOS), and subsequently by most western countries, including Israel.
MELD Score is a logarithmic formula that calculates the degree of severity of the liver disease and the chances of survival without transplant. The score ranges from 6 upwards. The severer the disease - the higher is the score. The registration of adults for liver transplant is conditional upon a MELD Score of 10 or more at the time of registration; if, after registration, the score goes down below 10, the patient shall not be removed from the list.
Liver allocation to children
Children up to age 18 are registered in a special children's list and are classified according to the severity of the disease in line with a system which distinguishes children up to age 12 from children above age 12.
Children up to age 12: The severity of the disease is calculated according to the PELD Score (PELD = Pediatric End-Stage Liver Disease), an arithmetic formula based on the same principles as the allocation model for adults, with additional parameters being taken into account in children due to the growth process: height, weight, age, and date of registration on the national waiting list.
The score ranges from 6 to 40. The severer the disease - the higher is the score.
Children aged 12–18 are included in the children's list, but the severity of the disease is calculated based on the MELD model used for adults.
Waiting List
There are two waiting lists, one for adults and one for children (up to age 18). There is no age limit for liver transplants.
Both lists are based on a score consistent with the severity of the disease and identicalness of the blood type. There is a difference in the formulas for the calculation of the severity of the disease in children and in adults, due to disease and age-specific characteristics. The match of the body sizes of the donor and of the recipient is taken into account. In each category there is a separate list for emergency cases – Status 1 – including patients with acute and hyper-acute liver disease (according to fixed criteria), hospitalized in a critical state, whose life expectancy – without transplant – is up to 7 days.
Allocation Model
- In the first place, the liver shall be allocated to a Status 1 emergency case candidate, based on identical or matching blood type.
- .If there is no Status 1 patient, the liver shall be allocated to a patient with a blood type identical to that of the donor and with the highest score, i.e. with the highest degree of severity of the disease.
- In exceptionally severe cases, with a MELD Score above 30 and with a rare blood type, the possibility shall be given for receiving transplants also from donors with matching (rather than only identical) blood type.
Kidney Allocation
Principles
In kidney allocation there is no emergency criterion.
The categorization of kidneys for transplant is based on identicalness of the blood types (O to O, B to B, etc.) of the donor and of the recipient.
Principles of allocation of kidney and pancreas (for type 1 diabetes patients)
- Match according to identicalness of blood types.
- 1.Negative cross-matching between the blood cells of the candidate and the blood cells of the donor, and according to seniority on the waiting list (there is a separate list for diabetes patients waiting for kidney + pancreas).
Waiting List
There is no age limit for kidney transplants. As a rule, registration for transplant from a deceased donor is possible only after the inception of dialysis therapy. When a patient is registered for transplant, the waiting period shall be calculated as of the date of inception of the dialysis therapy (rather than as of the date of registration for transplant).
A dialysis patient, who entered the waiting list at a certain age and due to prolonged waiting has "outgrown" the age group, shall continue to be granted the score in accordance with the age group to which he/she belonged at the moment of registration (the younger the candidate – the higher is the score granted).
Allocation Model
When a kidney donation is received, glands from the body of the donor are sampled and transferred to the National Laboratory for Tissue Categorization. The Laboratory keeps blood samples of all kidney and kidney-pancreas transplant candidates (the samples are sent to the laboratory once in a month). From the glands, cells are produced, which are examined against the blood samples of the candidates with the same blood type as the donor. This test is called "cross-matching". Only candidates in whom the cross-matching of the blood cells with the cells of the donor is negative can receive a kidney or a kidney and pancreas from the respective donor. Among the candidates with negative cross-matching, priority is established according to four criteria: age, waiting period (counted in months since the inception of the dialysis therapy), genetic compatibility (HLA) and level of antibodies (PRA). For each criterion there is a score varying between 0 and 4 points, except for the level of antibodies (PRA), where the score varies between 0 and 6 points. In the tables hereunder, the scoring method is presented. Some of the candidates have a high level of antibodies. This means that they have antibodies against numerous people and that their chances of finding a match with a kidney donor are low. In order to compensate for their low chances in finding a kidney, the Transplant Center determined a "higher" score for candidates with high levels of antibodies. In all cases of candidates with negative cross-matching with the donor, the total score is calculated, and the candidate with the highest score receives the organ.
Special cases:
- If the donor is a child below 18 years of age: a match shall be sought first among candidates that are children below 18 years of age.
- If the donor is above 60 years of age: patients above 60 years of age shall receive the transplant.
Criteria and score tables for kidney allocation:
1. Age
| 0-18 | 4 points |
| 19-40 | 2 points |
| 41-60 | 1 point |
| over 60 | 0 points |
2. Level of antibodies (PRA)
| 0-25% | 0 points |
| 26-50% | 2 points |
| 51-75% | 4 points |
| 76%+ | 6 points |
3. Waiting period
| up to 24 months | 0 points |
| 25-48 months | 2 points |
| 49-96 months | 2 points |
| 97+ months | 4 points |
4. Genetic compatibility (HLA)
| No incompatibility | 4 points |
| Incompatibility on one site | 3 points |
| No incompatibility on the DR site Incompatibility on other sites |
2 points |
Blood type match tables ("matching blood type")
|
A person with |
Can receive |
Can donate |
| O | O | O,A,B,AB |
| A | A,O | A,AB |
| B | B,O | B,AB |
| AB | O,A,B,AB | AB |


